Using U.S. taxpayer dollars, researchers at two universities are identifying older people behind on their recommended vaccines and testing personalized “nudges” to coax them into getting more shots. nih-nudge-more-vaccines-feature.jpg
According to grant documents obtained by Children’s Health Defense (CHD) via a Freedom of Information Act (FOIA) request, the National Institutes of Health (NIH) is funding the $2.2 million “BE IMMUNE” clinical trial, which began in 2020 and will run through 2025.
Researchers at the University of Pennsylvania and the University of Washington are using Electronic Health Records (EHR) data — the electronic records from doctors’ offices containing patients’ detailed health and demographic data — to target African American, Hispanic and Asian people with lower flu, pneumococcal and herpes zoster vaccination rates.
The ongoing study blames the “poor vaccination rates” on patients’ and clinicians’ “widespread decision-making biases.” The trial is testing strategies drawn from behavioral economics, which uses insights from psychology to understand — and in this case to “nudge” or direct — people’s decision-making behavior.
The randomized controlled study is headed up by Dr. Shivan Mehta and a team of healthcare management experts who combine medical and business-based strategies to run studies like these.
The trials often are based in Penn Medicine’s in-house “Nudge Unit,” where behavioral design teams are dedicated to figuring out how to influence patient choices.
The grant is part of a massive initiative by the NIH to increase vaccine uptake by changing how people make decisions. The initiative has included hundreds of millions of dollars in grants since 2020 to create “culturally tailored” pro-vaccine materials to promote COVID-19 and flu vaccines.
It also included more than 50 grants worth $40 million designed to increase HPV vaccine uptake.
Testing the ‘ladder’ of behavioral interventions
The study is testing different “nudges” at more than 100 primary care practices at Penn Medicine, University of Washington Medicine and the Veterans Affairs Health System, one of the world’s largest EHR vendors in the world.
Over 1,000 primary care physicians and thousands of eligible patients at those practices are involved in the trial.
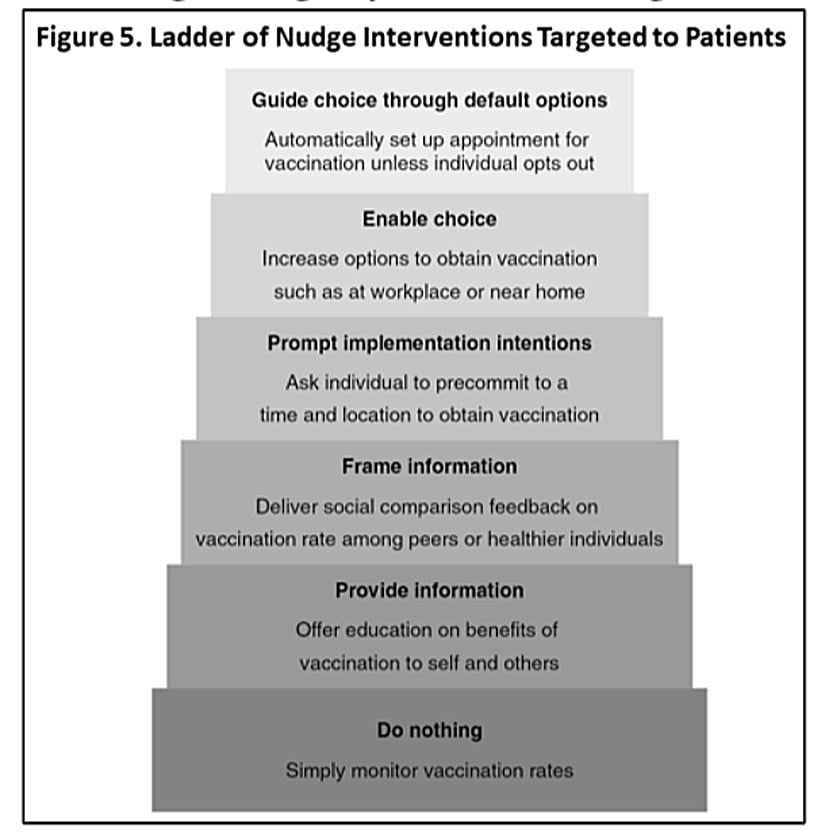
The range of tested interventions is scaled on a ladder.
Nudges lower on the ladder try presenting people with information so they can make their own decisions about vaccines —- methods that typically are not very effective for increasing vaccine uptake, the researchers said.
Nudges higher on the ladder either prompt people to make decisions, or simply plan their decisions for them.
For example, one nudge automatically sets up vaccination appointments for people, compelling them to go to their appointment and get vaccinated unless they intentionally opt out.
The “opt-out” framework has been effective in other areas of healthcare, such as colorectal cancer screening or persuading more people to take their flu shots, the researchers reported.
Netflix uses prompts to encourage binge-watching — healthcare should prompt people to get more shots
Penn’s “Nudge Unit,” which bills itself as the “world’s first behavioral design team embedded within a health system,” houses the study, which is also being conducted in a similar unit at the University of Washington.
Economist Richard H. Thaler and legal scholar Cass R. Sunstein popularized nudging in their 2008 book, “Nudge: Improving Decisions About Health, Wealth, and Happiness” as a method to create a “choice architecture” designed to influence people’s behavior in a predictable way “but without restricting choice” — particularly for policies or measures that might otherwise be unpopular.
Penn launched its Nudge Unit in 2016, inspired by British Prime Minister David Cameron’s Nudge Unit, established in 2010 to shape citizen behavior in the United Kingdom — a strategy the Penn researchers thought should also be applied to healthcare.
Penn’s Nudge Unit founders argued in a 2018 New England Journal of Medicine article that healthcare should use the same strategies businesses use to influence consumer behavior.
For example, they said, airlines require consumers to actively choose whether to purchase trip insurance before they can buy a plane ticket. Netflix changed its default settings to automatically play the next episode in a TV series to encourage binge watching.
“Similar opportunities exist to direct clinicians and patients toward better health care in situations where there’s consensus about desired behaviors,” they wrote, citing effective drugs, vaccines and targeted therapies as examples.
The strategy is being implemented globally — management consulting firm McKinsey reported that about 400 “nudge units” had been established globally by 2021.
However, even the Bill & Melinda Gates Foundation-backed Gavi concedes, “the theory has its critics — detractors argue that nudges can be paternalistic, invasive, ideological, and coercive in ways that erode public trust.”
The researchers behind this study also found that often the nudge approach doesn’t work.
In those cases, they argue “a stronger intervention—a ‘shove’—may be needed.”
EHR — an opportunity to scale up the nudge
The researchers celebrated EHR for offering a unique opportunity to develop and rapidly scale up personalized nudges.
The records increasingly are used for research and clinical trial recruitment because they contain a wealth of data. And new technological tools now allow researchers to “mine, assimilate, analyze, link, reproduce and transmit information” gleaned from that data.
Twila Brase, a registered nurse and author of “Big Brother in the Exam Room: The Dangerous Truth about Electronic Health Records,” told The Defender most people think the privacy of their EHR is protected by the Health Insurance Portability and Accountability Act, better known as HIPPA — but that’s not the case.
HIPPA only guarantees your data will be secure as it is passed among the various entities that have access to it, including researchers, Brase said. And that access can be provided without your consent.
“Nowhere in the law does HIPPA give you control over your medical records,” she said.
Because the records contain massive amounts of personal information that can be used and linked in many different ways, researchers studying EHR-based research argue that the use of EHR also raises “pressing questions concerning privacy, confidentiality, and patient awareness.”
They say that the use of one’s EHR data for research reasons can be confusing or even impossible to opt out of because often the provision of healthcare is linked to accepting a policy allowing researchers to use EHRs.
And EHR research often operates on the same logic as the nudge — an “opt-out” approach where permission is assumed unless a patient explicitly indicates they want to revoke it.

